Acne And The Skin Barrier: What You Need To Know
If you have acne-prone skin, understanding the relationship between acne and the skin barrier plays a crucial role in managing the skin condition. Here’s everything I wish I knew before I spent months dealing with painful breakouts and money on products designed for acne, but didn’t quite work the way I hoped for.
Note: I am not a doctor. Everything in this post is purely informational and based on my personal experience. Please consult a doctor before trying any new products.
Table of Contents
What is the skin barrier?
The skin barrier is the outermost layer of your skin and acts like your skin’s protective shield, preventing water loss (keeps your skin hydrated), protecting against external aggressors (bacteria, viruses, allergens, pollution, chemicals, UV rays), and maintaining the skin’s pH.
Think of your skin barrier like a brick wall — the skin cells are the ‘bricks’ and the lipids (fats like ceramides and fatty acids) and proteins are ‘mortar’ that holds everything together.
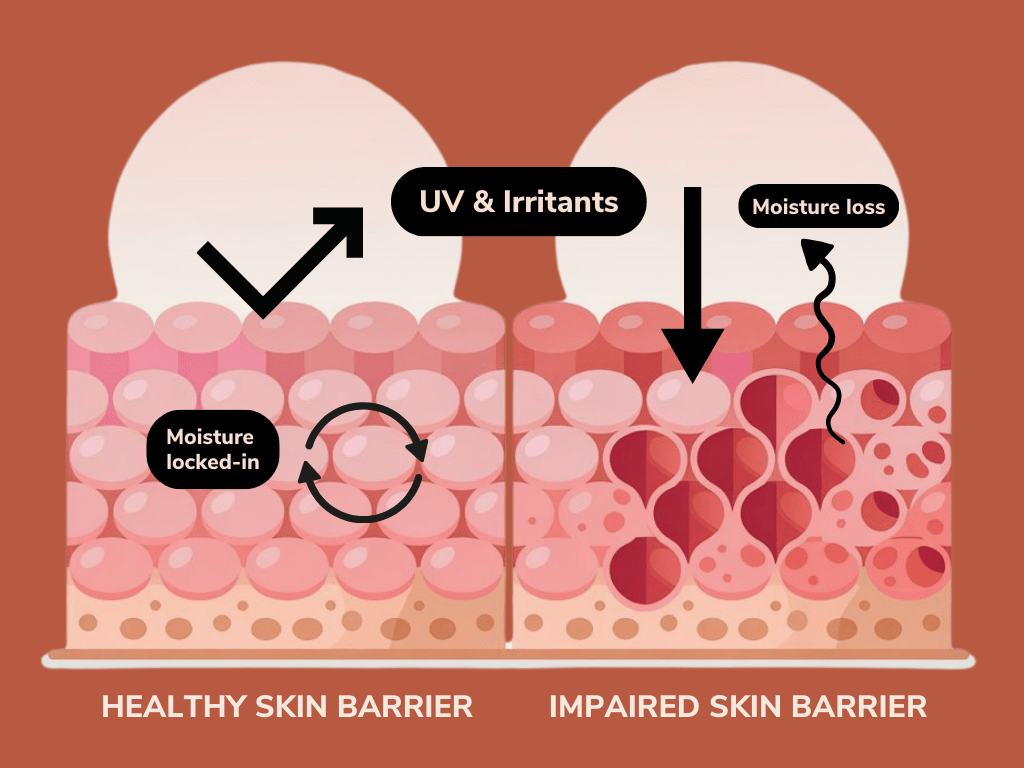
Healthy skin barrier vs impaired skin barrier
In a healthy skin barrier, skin cells are tightly packed and held together by lipids and proteins, forming a strong, protective layer that retains moisture and keeps out irritants, bacteria, and pollutants. These cells undergo a regular renewal process, where old cells are shed and new ones rise to the surface, maintaining a smooth, resilient texture.
In contrast, in an impaired skin barrier, skin cells may become damaged or improperly structured; they are less tightly packed together and therefore more permeable, aka ‘leaky’, leading to increased water loss and vulnerability to environmental stressors. This can result in dryness, irritation, redness, and a heightened risk of infection and acne breakouts.
Why understanding skin barrier function is important for acne-prone skin
Studies show that skin barrier function in acne-prone skin is ‘impaired’, so it’s important to know what role the skin barrier plays in both the development and worsening of acne.
Imbalanced oil production and abnormally composed sebum make the skin barrier more permeable to irritants and bacteria
Acne-prone skin often produces excess sebum, which contributes to increased chances of clogged pores (more on that below). The sebum is ‘abnormally composed’ with reduced levels of linoleic acid, a fatty acid essential for skin barrier integrity. Less linoleic acid means less lipid ‘mortar’ in the skin barrier, which makes the barrier more permeable (aka it has more ‘holes’), allowing irritants and bacteria to get in and trigger inflammation / breakouts.
Increased chances of clogged pores lead to acne lesions
Normal skin constantly produces new skin cells in the deeper layers of the skin, which move upward, mature, and eventually become part of the outermost layer. These outer cells are dead, flat, and filled with keratin (a protein in the skin), and over time, they are sloughed off through desquamation, which breaks down the proteins holding the dead skin cells together, making way for newer cells underneath.
To put it simply, in acne-prone skin, the shedding and renewal of skin cells is often dysregulated — if it’s too slow, meaning instead of being shed properly, dead skin cells can stick together with sebum, form a keratinous plug inside the follicle, and lead to clogged pores. If clogged pores aren’t cleared out fast enough, it leads to the buildup of keratin in the hair follicles, forming micrcomedones (the invisible beginning of an acne lesion), which can become open comedones (blackheads) or closed comedones (whiteheads).
Increased risk of dehydrated skin further worsens barrier function
Since the skin barrier is more permeable in acne-prone skin, there is a higher chance of water loss from the skin. This is known as Transepidermal Water Loss (TEWL), and causes:
- Disrupted skin barrier structure. Remember the brick and mortar analogy, in this scenario, imagine the mortar is drying out and crumbling.
- Dehydrated skin cells. Water is crucial for enzyme activity in skin cells for the healthy turnover, but low hydration causes the enzymes to malfunction, leading to the buildup of flaky or rough skin.
Interestingly, even oily (and acne-prone) skin types can be dehydrated, if it is not properly hydrated through consumption and skin care. If the skin is dehydrated, it compensates with more oil production to hydrate the skin, which can lead to breakouts.
Dehydrated vs dry skin
Dry skin is a skin type that lacks oil (sebum), often due to genetics, and feels rough, flaky, or tight. It needs rich moisturizers to restore softness and protect the barrier. In contrast, dehydrated skin is a temporary condition caused by a lack of water, often triggered by weather, harsh products, or over-exfoliation. It can affect any skin type, including oily, and may feel tight, look dull, and show fine lines, and needs gentle moisturizers and hydrating skincare to lock in moisture.
Chronic inflammation in the skin can cause the spread of acne lesions
When the skin barrier is compromised, it becomes more vulnerable to external irritants, including C. acnes (the bacteria associated with acne), to penetrate more easily into the skin, activating the immune system and triggering inflammation. This creates a vicious cycle because inflammation can damage the barrier and cause the spread of acne lesions.
Skincare actives and acne treatments exacerbate barrier damage
Given that the barrier function in acne-prone skin is impaired to begin with, it’s important to be careful when using common treatments recommended for acne, like benzoyl peroxide, salicylic acid, retinoids, and exfoliants, because they can be harsh.
Products for acne are designed to unclog pores and promote cell turnover. However, when this happens too fast, the skin doesn’t have enough time to properly form a strong, cohesive barrier. This can lead to a weakened skin barrier, causing dryness, flakiness, irritation, and increased sensitivity. The rapid turnover also means that skin cells may be immature and not fully equipped to hold moisture or protect against external irritants, which can result in redness, peeling, and even breakouts.
Maintaining a healthy skin barrier can help prevent acne
Knowing what we know about the relationship between acne and the skin barrier, the main objective of a skincare routine for simple acne cases should focus primarily on maintaining a healthy skin barrier.
Tips for skin barrier support and repair:
- Use gentle face cleansers
- Avoid over-exfoliating, especially no physical scrubs
- Moisturize day and night with barrier-supporting ingredients (ceramides, hyaluronic acid, niacinamide)
- Use a hydrating toner and/or essence in PM routine — the extra hydration is key!
- Wear sunscreen daily
- Avoid hot water and harsh treatments
- Use skincare actives such as retinol and salicylic acid with guidance from a doctor
For severe acne, consult a doctor.
Related:
Affordable Skincare Routine To Soothe and Reduce Acne Redness
Best Sunscreens For Acne-Prone Skin With No White Cast
Before and after photos of acne breakout following skin barrier routine
Here’s a before and after of my skin 4 weeks apart, following the skin barrier skincare routine below to heal a severe breakout.
AM routine: Vitamin C, moisturizer rich in ceramides, and sunscreen
PM routine: double cleanse (oil cleanser + gentle facial cleanser), hypochlorous acid toner, hydrating essence, and moisturizer rich in ceramides
In the before photo, my skin barrier is visibly unhealthy. It looks dull, dehydrated, and is inflamed, red, and itchy with small pimples popping up constantly. In the after photo, even though there is quite a bit of post-inflammatory pigmentation from the acne scars, the quality of my skin overall is so much smoother, radiant, and plump, and new breakouts stopped happening.


Final thoughts…
After more than two decades of dealing with acne and a decade of trial, error, and research on how to take care of it, I finally learned that the first place to start with care for acne-prone skin before, during, and after breakouts is always the skin barrier.
If the skin barrier isn’t well supported, skincare products, especially with actives, are going to do more harm than healing. Don’t fall into the trap of trying the instant fix products or routines.
Acne is considered a chronic inflammatory skin disease, and I haven’t found an explanation for why and how it happens that is simple and easy to digest. So, I hope this post explains what I wish I knew about acne right at the beginning of this journey, because it has completely changed my perspective on living with and managing the condition.